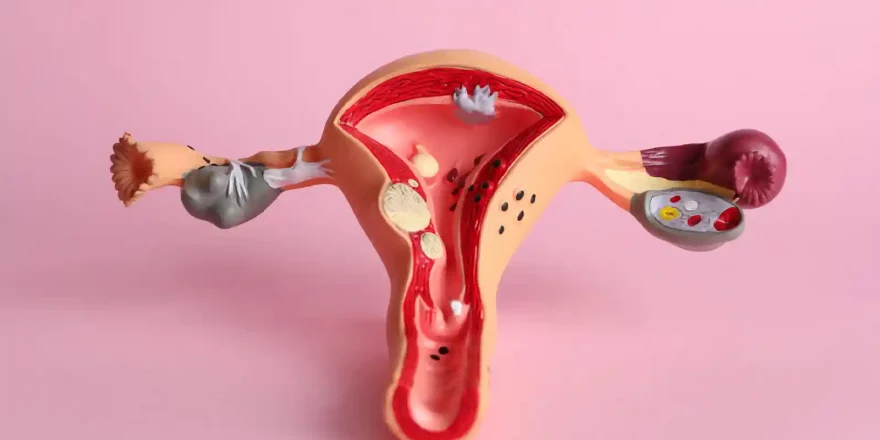
Low hormone levels prevent regular ovulation for many women and is a condition termed “hypogonadotrophic hypogonadism”, which means “low sex hormone levels causing sex organs to under-function. The menstrual cycle relies on the release of hormones from three glands to function, and a lack of hormones from any of them reduces the chances of conceiving and the health of a pregnancy if there is one. Hypogonadotrophic hypogonadism can affect both sexes and is sometimes linked to low body weight. The three glands are:
- The hypothalamus releases GnRH, and this stimulates the anterior pituitary
- The anterior pituitary in the brain releases the hormones FSH and LH, which:
- Stimulate the ovaries to recruit eggs to new cycles
- Trigger the release of an egg at ovulation
- Stimulates sex hormone production by the ovaries
- The ovaries produce estrogens and progesterone, which control the cycle
When the levels of FSH and LH are too low to stimulate the ovaries, menstrual cycles stop or fail to function healthily. With men, there is a fall in their sperm counts and sex hormone production.
- Women experience low levels of Follicle Stimulating Hormone (FSH) and Luteinizing Hormone (LH)
- Menstrual cycles and periods stop due to “hypogonadotrophic amenorrhea” (low sex hormone levels causing periods to stop)
The production of sex hormones varies during our lives:
- Sex hormones are activated a couple of months after conception (while the baby’s in the womb) and stay active for a few months after birth
- Sex hormone production then “shuts down” until puberty while the body grows and develops
- When girls reach a size and age that can accommodate pregnancy, the sex hormones reactivate, and the body is altered into a reproductive state
- The production of sex hormones from the ovaries decreases as women approach menopause (also true for men as they approach andropause)
Causes

There are two leading causes of low sex hormones:
- During times of severe stress, the hypothalamus (the junction between the hormonal and nervous system) naturally suppresses sex hormones
- Malnourishment leads to a deficiency of the nutrients and fats needed to make hormones
The body will naturally prioritise survival rather than pregnancy when energy levels are critically low, and sex hormone levels are usually an issue when:
- The person is underweight (BMI under 19)
- Over-exercising (say running marathons) is a common cause as exercise reduces fat, cholesterol, and the energy levels needed for menstrual cycles (exercise and fertility)
- Severe “stress” can disrupt the hypothalamic-pituitary-gonadal (HPG) axis and the release of hormones that stimulate the ovaries (emotions and fertility)
- Very low-fat diets, as cholesterol is essential for hormone production
- Rare genetic conditions such as Kallman’s or Sheehan’s syndrome (defects in around ten genes can cause this) i
Background information
- Cholesterol is essential to make sex hormones and steroids, and low cholesterol levels can reduce sex hormone levels
- Low LH and FSH levels can’t stimulate the ovaries enough to recruit eggs to new cycles or release mature eggs at ovulation
- Estrogen stimulates the growth of the womb lining, and low estrogen causes a lining that’s too thin for successful implantation
- Women in this situation often have a bleed every six weeks or so when the womb lining spontaneously breaks down
Diagnosis
- Blood tests will show low LH, FSH, and estradiol levels in hypogonadotropic hypogonadism, regardless of the underlying cause
- A health history (including a general medical check-up, BMI measurement, exercise and eating habits) helps reveal the cause
- Specialist genetic testing is needed for genetic causes
Treatment options
- Weight gain is essential for people with low BMI
- A diet with enough saturated fats
- A reduction in exercise if over-exercising is part of the problem
- A gonadotrophin (GnRH) releasing hormone pump is needed in some cases
Photo by Testalize.me on Unsplash