There are different types of polycystic ovaries, and which type a woman has makes a huge difference to her chances of conceiving. Millions of women have polycystic ovaries, but they don’t all have fertility issues because it can be perfectly normal for them to have many large follicles in their ovaries (the “cysts”).
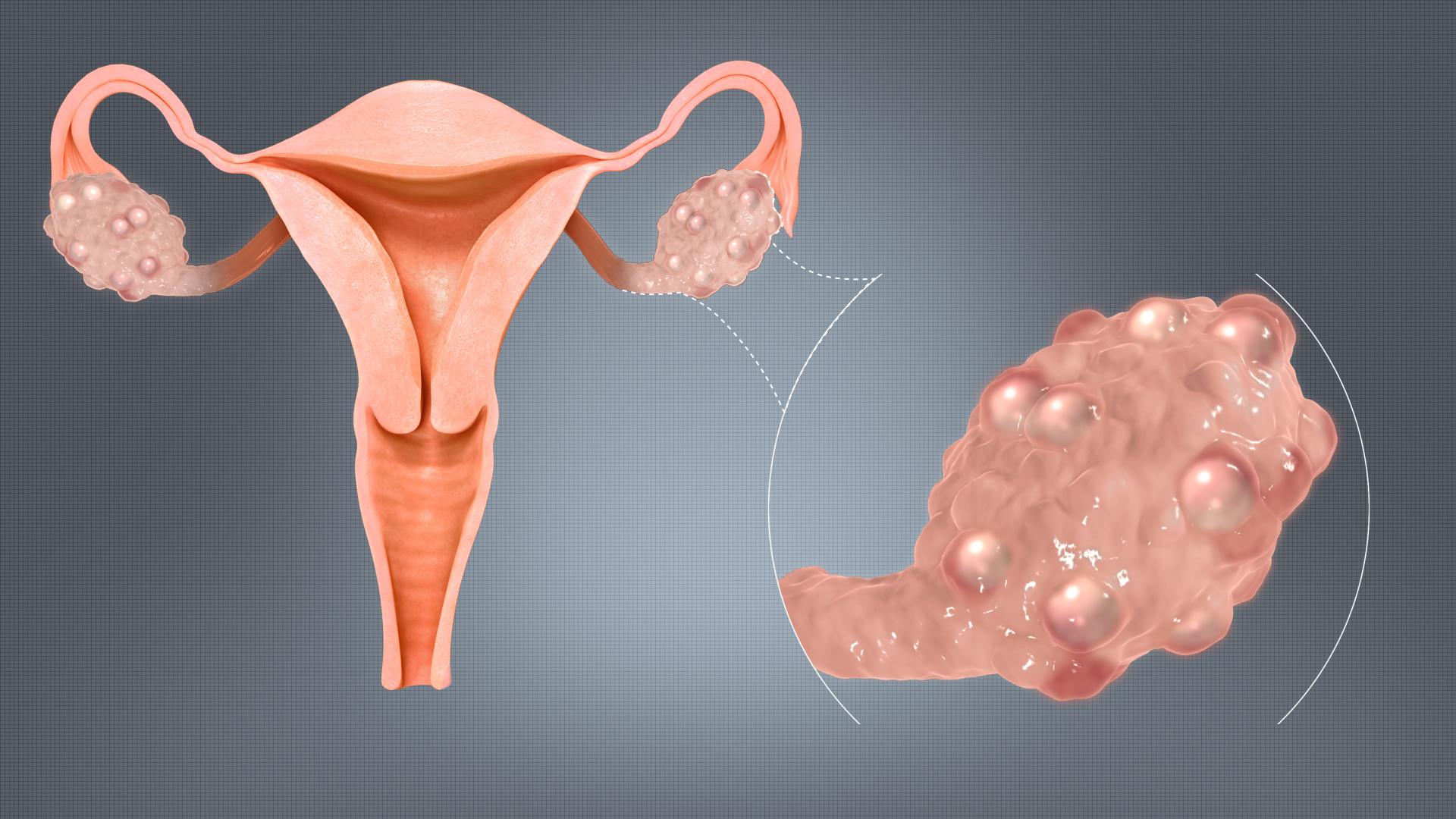
The problem as far as conceiving is the number of follicles, their size, and what they’re doing. To explain; in healthy menstrual cycles, the ovaries contain many follicles of a variety of sizes:
- Each cycle, the biggest “dominant” follicle releases an egg at ovulation
- The ruptured ‘“dominant” follicle becomes the corpus luteum In the luteal phase
- The other large follicles that grew alongside the ‘“dominant’” follicle are re-absorbed into the ovary
- If the other large follicles remain, or if the dominant follicle doesn’t rupture, the ovaries become “polycystic”
Polycystic ovaries
There are three “polycystic ovary” terms, all involving many large follicles in ovaries:
- Polycystic ovaries (PCO)
- Polycystic ovary morphology (PCOM)
- Polycystic ovary syndrome (PCOS)
Polycystic ovaries (PCO) and polycystic ovary morphology (PCOM) mean the same thing as ‘morphology’ simply means “form and structure”. They describe ovaries of abnormal size, shape and number of follicles, and the criteria are:
- Ovaries are over twice the usual size
- They have follicles around the edge that look like a “string of pearls” on ultrasound
- The centre of the ovary produces a bright echo on ultrasound
PCO/PCOM may be a variation of the norm that doesn’t affect fertility as:
- About 33% of women with regular menstrual cycles have PCO
- The proportion of women with PCO falls with age
- Women with PCO have higher anti-Mullerian hormone (AMH) levels and lower follicle-stimulating hormone (FSH) levels
- Not all women with PCO have the hormonal and metabolic abnormalities seen in PCOS
This is important as young women diagnosed with PCO/PCOM could be as fertile as the next woman, and the number of large follicles in their ovaries may naturally reduce with age.
However, lifestyle has a powerful influence, and obese girls with PCO are 2.5x more likely to develop PCOS. This is because obese girls are more likely to have high insulin levels and develop metabolic syndrome, which are powerful drivers of PCOS.
Polycystic ovary syndrome (PCOS)
PCOS differs from PCO/PCOM because it has a significant impact on monthly conception rates and sex hormones. The ovaries of women with PCOS are stimulated to release excess male hormones (testosterone), which changes the nature of the menstrual cycles:
- Follicles growing in the follicular phase release estrogens
- The corpus luteum that develops from the dominant follicle releases progesterone
- When follicles become “cysts”, they release more of the male hormone testosterone
Men and women have exactly the same sex hormones, and they’re all essential for healthy eggs and sperm. However, the balance and level of sex hormones vary significantly between the sexes, and they change with age.
In PCOS, the abnormally high testosterone level encourages many large follicles in the ovaries and prevents ovulation.
- PCOS is the most common cause of infertility due to non-ovulation
- About a third of couples attending infertility clinics have ovulation issues, and PCOS is the cause of 70-90% of these cases iii
- Between 5% and 10% of women are thought to have PCOS worldwide
- Rates are highest in industrialised countries, and PCOS affects about 20% of women in the UK iv
- About 25% of couples going to fertility clinics have PCOS, and the reason is eggs are rarely (or never ovulated), making conceiving almost impossible
i ‘Updated ultrasound criteria for polycystic ovary syndrome: reliable thresholds for elevated follicle population and ovarian volume.’ Lujan ME, et al. Hum Reprod. 2013 Mar 15
ii Tsan-HonLiou et al. “Clinical and biochemical presentations of polycystic ovary syndrome among obese and nonobese women” Fertility and Sterility Volume 92, Issue 6, December 2009, Pages 1960-1965
iii ‘What is polycystic ovary syndrome? Are national views important?’ Balen A, Michelmore K. Hum Reprod. 2002 Sep; 17(9):2219-27.
iv “The Prevalence and Features of the Polycystic Ovary Syndrome in an Unselected Population”. Azziz R, Woods KS, Reyna R, Key TJ, Knochenhauer ES, Yildiz BO (June 2004). Journal of Clinical Endocrinology & Metabolism 89 (6): 2745–9.