PCOS Treatments
There are three main approaches to the treatment of PolyCystic Ovary Syndrome (PCOS), based on :
- Weight loss.
- Western medication or surgery.
- Complementary therapies, including supplements.
(i) Weight loss
The chances of having PCOS increases with weight, which makes weight loss the first line of treatment for most women with PCOS. Weight loss can dramatically change hormone levels to improve fertility and reduce other health conditions, including diabetes, hypertension and high cholesterol.
Losing just 5% of your body weight usually alters hormone balance enough to normalize ovulation and make natural pregnancy possible. When women lose 10% of their body weight, it reduces the fat in the body by 30%. When this happens, nearly every woman ovulates normally! i For women of 180lbs, that’s just a 9lbs reduction.
The good news is that when obese women with PCOS follow a[show_to accesslevel=” premium” no_access=’
‘] 1200 kcal/day diet this happens:
- Three quarters lose 5% of their weight, and a third lose 10%.
- All reduce their BMI, body fat and waist and hip circumferences.
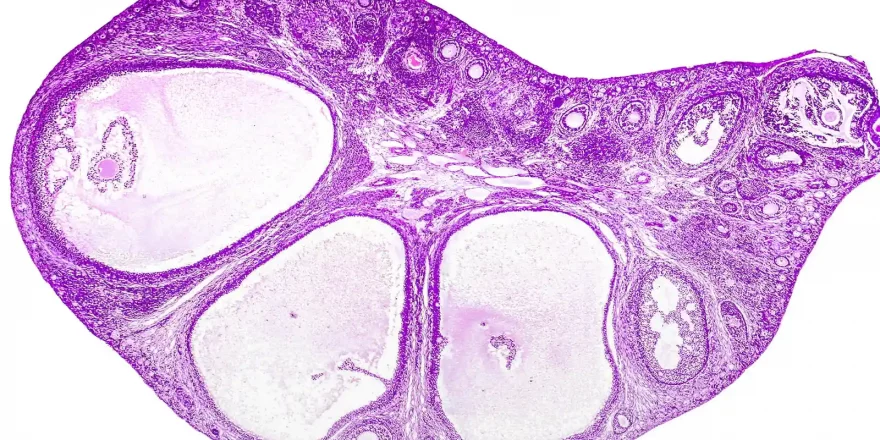
- The ovaries significantly shrink in size, as do the number of cysts in them.
- Two-thirds of non-ovulating women resume regular cycles.
- A third get pregnant when they lose at least 5% of their weight.
PCOS stems from problems with sugar metabolism and insulin resistance for many women (including many average weight women). The reason for this is that high insulin levels stimulate the ovaries to produce testosterone. Genetics and the environment contribute to PCOS, and some people are more prone to insulin resistance than others on the same diet. This is simply because their ancestors had become well adapted to low carb and sugar diets.
Diet is a tricky subject, and the best way to lose weight usually involves joining a support group, cutting calories (especially sugar) and taking regular exercise at the same time. The relationship between PCOS and high insulin levels makes a diabetic-type diet ideal, but also bear in mind that:
- Increasing protein in the diet reduces PCOS rates (we strongly advise vegetable protein) ii
- A high-fat diet contributes to PCOS (and insulin resistance) developing iii
- A low carb diet reduces PCOS (and insulin resistance) iv
- Losing weight by dieting is far more effective than taking metformin type drugs for obese and overweight women with insulin resistance and PCOS v
There’s more information on weight and fertility in lifestyle and types that are personal, effective and inexpensive.
(ii) Medication
Doctors often suggest drugs for PCOS. The usual is birth control pills as they offer more regular periods and less hair growth. Still, they do stop you from having a baby…! Women trying to conceive and wanting a medicated answer are best off seeing a reproductive endocrinologist for a proper evaluation. The treatment they’ll usually recommend is:
- Clomiphene citrate (clomid)vi is inexpensive and often successful, especially for younger women. We think it’s less appropriate for Tired or older women as it thins the womb lining, which can be an issue for them. Clomid also carries a risk of ovarian hyper-stimulation syndrome (OHSS). The side effects including hot flushes, mood swings, visual disturbances, breast tenderness, nausea and pelvic discomfort. Natural alternatives to clomid include black cohosh, and they avoid the side effects. If clomid doesn’t do the trick, the options are then usually:
- Gonadotropins are hormones that directly affect the ovaries (usually FSH). These are expensive and increase the risk of multiple pregnancies and ovarian hyper-stimulation syndrome (OHSS), so a low-dose regimen with ultrasound monitoring is usually offered. vii
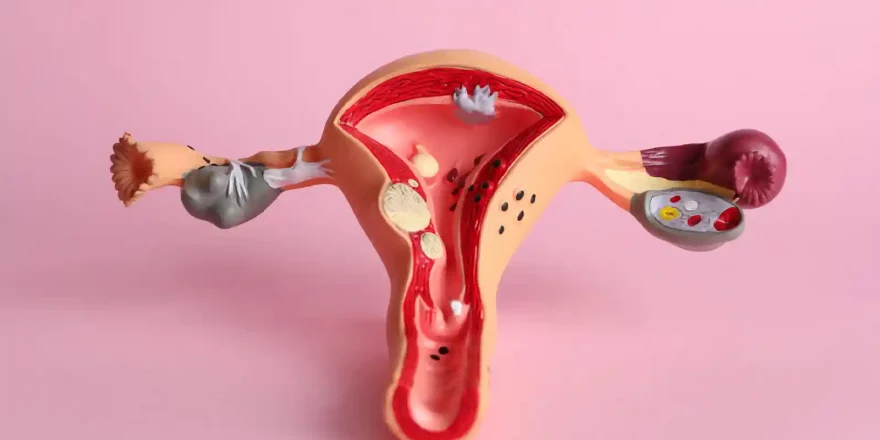
- Ovarian drilling involves laparoscopic surgery where 4-10 small follicles are punctured and often triggers normal ovulation or ovulation along with Clomid or FSH. However, it also destroys ovarian tissue and reduces ovarian reserve.
- Metformin is often prescribed alongside clomid for women with PCOS. The guidelines for metformin use in PCOS advise restricting it to women with glucose intolerance. There’s some debate about its routine use for PCOS, and there are viable, healthy alternatives. viii
(iii) Supplements and Complementary treatments
There’s some compelling evidence on complementary and supplements for treating PCOS: