Miscarriage is almost a taboo subject that’s rarely discussed because of the distress involved. It’s usually only after a personal experience that people discover just how many of their friends and family have been there too. It’s believed that up to 50% of all pregnancies don’t progress, but most are very early on, and as the period is relatively on time, it’s not recognised. However, 10-15% of pregnancies are lost later on and are clearly miscarriages: i
- 80% are in the first 12 weeks
- 90% are in the first 16 weeks ii
An unfortunate 5% of couples have 2 consecutive miscarriages, and 1% of couples have 3 or more losses in a row, which is a condition called “recurrent miscarriage”. A miscarriage is deeply upsetting, but it’s reassuring to know that most couples (76%) get pregnant with a healthy baby within the year. iii
Signs of miscarriage
The signs of miscarriage are usually blood loss, cramping, and pain in the lower abdomen. If this happens, seek medical advice at the local hospital’s “early pregnancy unit”. However, it’s quite common for women to get light bleeding in the first 12 weeks of pregnancy, so bleeding doesn’t necessarily mean a miscarriage is happening. When a baby is lost after 20 weeks (or over 500g), the medical term is a “stillbirth”, but sometimes medics still use the term “spontaneous abortion” which can cause confusion and distress to the family.
Types of miscarriage
There are five different terms that apply to miscarriage:
- Threatened miscarriage usually involves mild symptoms of bleeding, usually with little or no pain, and the cervix is closed. A scan will show “hypo-echogenic” areas behind the gestational sac, and the risk of miscarriage is between 4-33%, depending on the stage of pregnancy
- Inevitable miscarriage involves heavy bleeding with clots and pain, the cervix is open, and the bleeding may be severe enough for the woman to collapse. Unfortunately, it’s impossible to save the pregnancy
- Missed miscarriage is when the fetus has died and is still held in the womb, but pregnancy tests can remain positive for several days. The symptoms of pregnancy have usually decreased or gone, and a persistent dirty, brown discharge may appear. Ultrasound scans show there’s no fetal heartbeat
- Incomplete miscarriage is a situation in which heavy bleeding has occurred, and the miscarriage has been confirmed, but “retained products of conception” (either the amniotic sac or placenta) remain in the womb
- Recurrent miscarriage is the term used for the condition when a couple has had three or more consecutive losses
When couples experience a second miscarriage, consider preserving some of the tissue lost (in contact lens solution) for chromosomal testing. Miscarriages due to abnormal chromosomes usually have little bearing on future pregnancies, and if the chromosomes are OK, it indicates other investigations are needed. Couples having IVF often choose to have preimplantation genetic diagnosis (PGD) testing to avoid chromosomal issues.
Causes of miscarriage
The risk of a miscarriage varies with age, lifestyle, health history and immune state. The ten main causes of miscarriage are:
- Chromosomal abnormalities
- Placental problems
- Thrombophilia
- Immune issues
- Antibiotic use
- Abnormalities of the uterus or cervix
- Hormonal abnormalities
- Lifestyle choices (cigarettes, alcohol, coffee, drugs)
- Bacterial infections
- Polycystic ovary syndrome (PCOS)
1. Chromosomal abnormalities
- Extra or missing chromosomes create a condition called “aneuploidy”, and any fetus with extra or fewer than the standard 46 chromosomes has such significant problems that it usually ends in miscarriage. Aneuploidy is due to random errors in eggs or sperm that everyone produces, and some babies are born with aneuploidy variations, such as Downs Syndrome (three of chromosome 21)
- DNA fragmentation is when bits of genetic material on the chromosomes get broken off and misplaced. Fragmentation happens to DNA in all eggs and sperm, but the greater the damage, the more difficult it becomes for the embryo to repair and fill in the missing material. Implantation is usually fine, but as the cells divide and replicate, the organisation within the cells decreases and the pregnancy becomes less and less viable. DNA fragmentation rates typically get higher with age and exposure to toxins, and while standard chromosome testing doesn’t detect DNA fragmentation, sperm can be tested.
2. The placenta
The placenta is the vital link between mother and baby, and it develops from the outer ring of cells of the embryo at the blastocyst stage. If there are problems with the implantation site and or with how these cells develop, it can lead to miscarriage. The placenta also takes over progesterone production from the corpus luteum towards the end of the first trimester, and if this crucial shift is incomplete or poorly timed, it will cause low progesterone levels, and miscarriage will follow.
3. Thrombophilia
Thrombophilia is an increased tendency of the blood to clot, and it’s a significant cause of miscarriage as blood gets thicker in pregnancy anyway. Any blood clotting around the placenta reduces the supply of blood to the baby, which can quickly starve the baby of oxygen and nutrients.
Several conditions increase the likelihood of blood clotting, particularly antiphospholipid antibodies –APAs, and there are also associations with other antibodies (anticardiolipin (aCL), lupus anticoagulant (LAC) and anti-β2 glycoprotein I antibodies). Most causes of thrombophilia can be tested for relatively easily, and between 10-20% of women with early pregnancy loss reportedly test positive to APAs.
4. Immune issues
The immune system is crucial for health and pregnancy requires it to recognise it and make big changes. Immune imbalance has a central role in thrombophilia, and other immune conditions also increase the risk of miscarriage, including raised natural killer cells, raised antinuclear antibodies, reduced levels of leukocyte antibodies and systemic lupus erythematosus.
The immune system is also involved when women have subclinical infections and inflammations of the uterus, which involves high levels of cytokines that themselves encourage further immune activity. iv Fortunately, there’s a growing range of tests and treatments for some of these conditions, and they’re becoming more accessible.
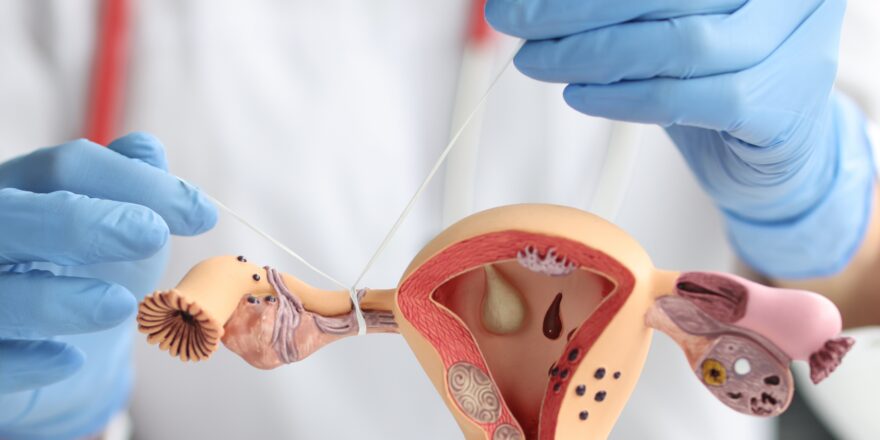
5. Anatomy of the uterus
An abnormal structure of the uterus or cervix can increase the likelihood of miscarriage and is thought to cause 10% of cases, and a divided septum in the womb is the usual cause. The septum is a normal part of uterine development and is usually re-absorbed as a girl develops in the womb. However, sometimes it’s not completely re-absorbed, which causes a division down the centre of the womb, but surgery can easily correct it.
A weak or incompetent cervix can struggle to retain a pregnancy in place once the baby gets bigger (towards the end of the first trimester), and surgery (cerclage) to stitch the cervix closed is usually needed. For some women, fibroids (myomas) and polyps in their womb can also cause problems, and in all, about 15% of women who have recurrent pregnancy loss it’s because of an anatomical problem. v
6. Antibiotics
It’s not uncommon for antibiotics to be given in pregnancy, especially for urinary tract infections (UTI), but unfortunately, they can significantly increase the chances of miscarriage if they’re taken in the first trimester. If you’ve been advised to take antibiotics, it’s best to contact your medic as these types are associated with an increased risk of miscarriage compared to penicillins, cephalosporins or no antibiotics at all. vi
- Macrolides (except erythromycin)
- Quinolones
- Tetracyclines
- Sulfonamides
- Metronidazoles)
7. Hormonal issues
Hormones play a crucial role in pregnancy, and a high level of progesterone is essential to stay pregnant; however, some other hormones can increase the chances of miscarriage when they’re abnormal:
- Thyroid disorders, especially low thyroid hormone levels, increase the risk of miscarriage in early pregnancy. vi It’s recommended that women wishing to get pregnant who are being treated for hypothyroidism should have their thyroxin dose adjusted before trying to conceive viii
- Diabetes is another hormonal issue that affects fertility and pregnancy, and it carries a significantly increased risk of miscarriage or stillbirth (2.5x). Overall the average medical cost for managing the pregnancy of a woman with diabetes is almost double the norm ix
8. Lifestyle
Lifestyle choices have significant consequences on the chances of getting pregnant and for staying pregnant. Drugs, alcohol, cigarettes, coffee, environmental toxins and exercise (too much/too little) all affect the chances of miscarriage, and unhealthy lifestyles are linked to around 10% of fetal abnormalities.
9. Bacterial infections
Infections and imbalances of the womb microbiome can increase the chances of miscarriage, and Mycoplasma hominis and Ureaplasma urealyticum are the main causes as they can inflame the womb lining and interfere with the function of the placenta. Bacteria (including these) are a normal (and essential) part of the womb environment, but when the balance of the community is radically altered, it can affect the health of the womb.
Women with unexplained infertility have higher levels of undiagnosed vaginal infections (37.4%) than fertile women (15.4%), while 60.1% of women with PCOS have undetected infections. x
10. Polycystic ovary syndrome
PCOS is a condition with both hormonal and structural abnormalities that cause anovulation and reduce the chances of conceiving, but what’s less well known is that PCOS also appears to increase the risk of miscarriage and premature birth. The link is indirect and is due to an increased risk of developing cervical incompetence and due to PCOS having been closely connected to other hormonal conditions like Type II diabetes and metabolic syndrome. xi
iiTang OS, Ho PC. The use of misoprostol for early pregnancy failure. Curr Opin Obstet Gynecol. 2006;18:581-586
iiiHassan MAM, Killick SR: Is previous aberrant reproductive outcome predictive of subsequently reduced fecundity? Hum. Reprod.20(3),657–664 (2005).
ivJoining the Immunological Dots in Recurrent Miscarriage Bansal, A. S. (2010), American Journal of Reproductive Immunology
vPropst AM, Hill JA (2000). “Anatomic factors associated with recurrent pregnancy loss”. Semin. Reprod. Med.18 (4): 341–50. doi:10.1055/s-2000-13723. PMID11355792.
vi“Use of antibiotics during pregnancy and risk of spontaneous abortion” Flory T. Muanda, MD, Odile Sheehy, MSc, Anick Bérard, PhD. CMAJ May 1, 2017 vol. 189 no. 17 E625-E633
viiMaternal Subclinical Hypothyroidism and Thyroid Autoimmunity in Early Gestation Are Associated with Increased Risk of Miscarriage. Pearce Elizabeth N. Clinical Thyroidology. September 2014, 26(9): 235-237. doi:10.1089/ct.2014;26.235-237.
viiiLevothyroxine-Treated Women in Their Reproductive Years Should Have their Serum TSH Adjusted Before Conception to Prevent Hypothyroidism in the First Trimester. Mestman Jorge H. Clinical Thyroidology. October 2014, 26(10): 254-257. doi:10.1089/ct.2014;26.254-257.
ixJovanovič, L., Liang, Y., Weng, W., Hamilton, M., Chen, L., and Wintfeld, N. (2015) “Trends in the incidence of diabetes, its clinical sequelae, and associated costs in pregnancy“. Diabetes Metab Res Rev, 31: 707–716. doi: 10.1002/dmrr.2656.
x Bacterial vaginosis and infertility: cause or association?” Magdy AM. J Obstet Gynecol Reprod Biol. 2013
xi “Co-morbidity of cervical incompetence with polycystic ovarian syndrome (PCOS) negatively impacts prognosis: A retrospective analysis of 178 patients” Yongqing Wang Et al. BMC Pregnancy and Childbirth201616:308. DOI: 10.1186/s12884-016-1094-6