Investigations for anovulation are essential when deciding treatment choices, and as the main cause of female infertility is a lack of ovulation, these tests are crucial. In total, about 30-40% of couple infertility is female based; the same is true for men, with the rest being combined factors between the couple. However, about a third of couples that attend fertility clinics are affected by anovulation, and there are both hormonal and non-hormonal causes.
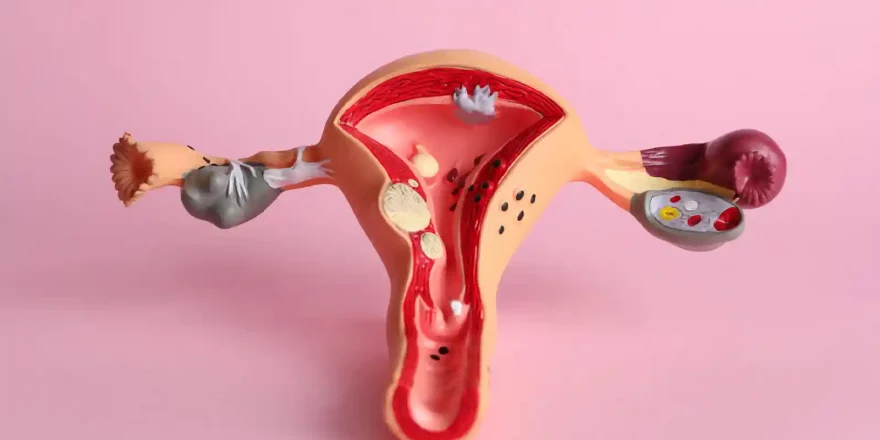
The three hormonal causes of anovulation are:
- Polycystic ovary syndrome (PCOS) is the main reason for anovulation, and it’s caused by abnormally high levels of male sex hormones (androgens)
- Hypogonadotrophic hypogonadism is a condition where abnormally low levels of sex hormones fail to trigger new cycles
- Hyperprolactinaemia involves high levels of the hormone that stimulates lactation (milk) and also prevents the start of new cycles
The three non-hormonal causes of anovulation are:
- LUFS, where the dominant follicle is “luteinised”, but the egg isn’t released, it can’t be fertilised, and a “functional cyst” develops
- Genetic conditions that alter the normal development of the ovaries
- Premature ovarian failure is the unexpectedly early arrival of menopause (before the age of 40)
morefertile® has extensive information on a wide range of conventional and complementary treatments for anovulation.
| Investigation | Appropriate timing | Interpretation |
|---|---|---|
| Progesterone | 7 days past ovulation; (e.g. Day 21 if ovulation was on day 14 in a 28-day cycle) |
|
| Follicle stimulating hormone
(FSH) |
Day 2-3 of the cycle |
|
|
Luteinising hormone (LH) |
Early in the follicular phase |
|
|
Testosterone |
Any time in the cycle |
|
|
Prolactin |
Any time in the cycle (but not after exercise or stress) |
Over 1000 IU/l indicates a pituitary adenoma; a repeated test will confirm this |
|
Thyroid stimulating hormone (TSH) |
Any time in the cycle if there are signs of hypothyroidism or hyperprolactinaemia |
High TSH indicates hypothyroidism |
|
Transvaginal ultrasound scan |
Oligomenorrhoea or amenorrhoea or raised LH or testosterone levels |
Identifies polycystic ovarian morphology |
| MRI/CT scan of the pituitary | If two prolactin levels are over 1000 IU/l | Identifies the presence of macroadenomas |
|
Karyotype |
Primary amenorrhoea (never) |
Identifies chromosomal abnormalities, translocations or HLA DQ alpha incompatibility between partners |
|
Body mass index (BMI) |
Oligomenorrhoea or amenorrhoea |
|