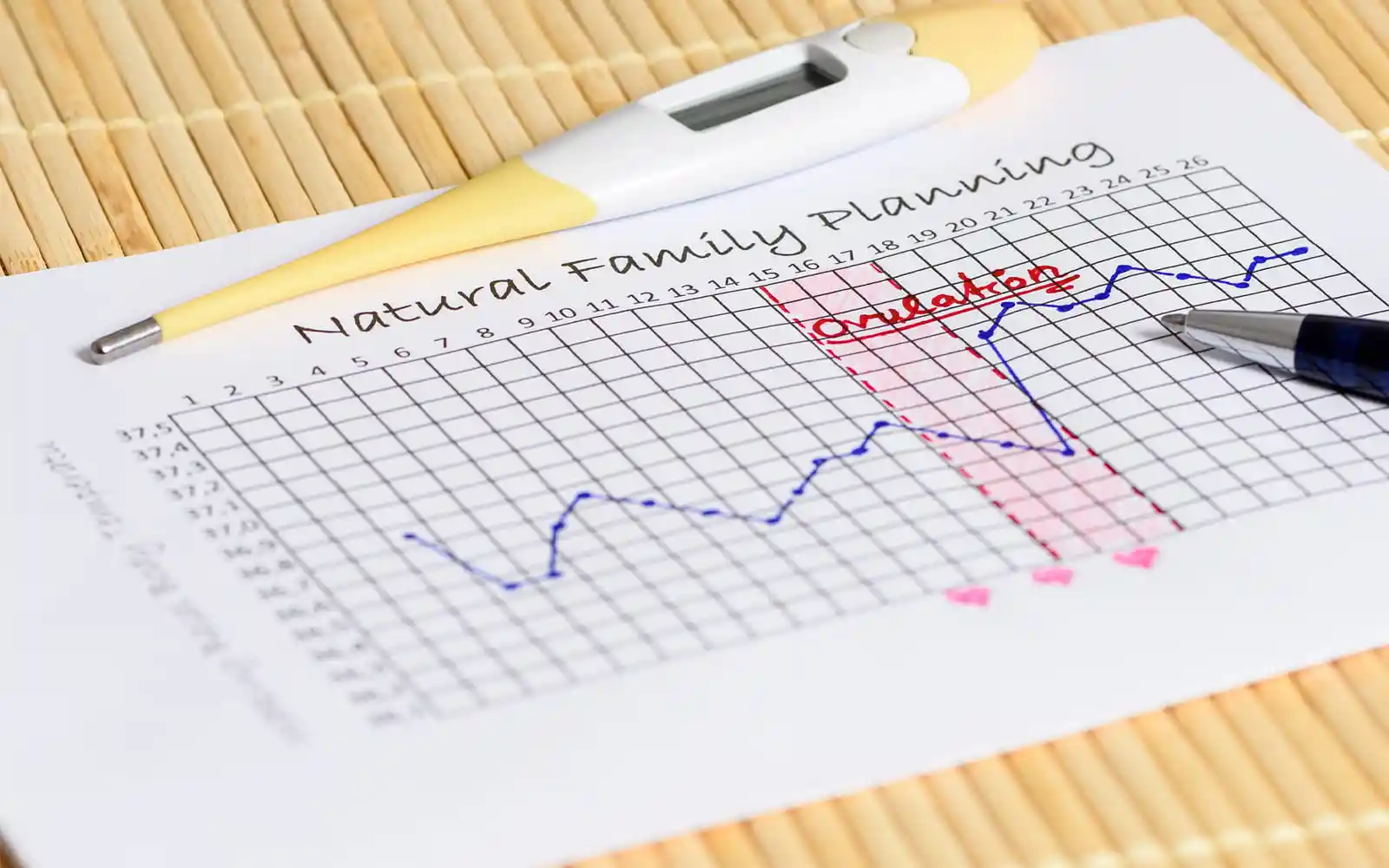
Basal body temperature charting (BBT) relies on two factors that change in response to female sex hormone levels. Temperature is one, and the other is changes in the cervix and the mucus it produces. Recording them gives a good indication of sex hormone levels and when ovulation probably occurred. The “golden rules” for taking BBT temperatures are:
- Day 1 of the cycle is the first day of waking with a period
- Temperatures must be taken on waking
- On broken nights an hour of rest or sleep is needed before taking the temperature
- The thermometer needs to be in place for 3 minutes
- Take the temperature the same way, either under the tongue or in the vagina
Things that affect accuracy:
- Changing the thermometer
- Where the thermometer is put
- When the temperature’s taken (about 0.1°C rise for each hour later)
- The environment (travel, holidays, climate)
- Stress and emotional stress
- Alcohol
- Eating big meals late
- Late nights or shift work
- Short or broken sleep
- Illnesses
- Some medications (esp. hormones and antihistamines)
Recording these factors helps decide if temperature “spikes” can be ignored or if they’re important.
It’s worth knowing
- These issues affect the follicular phase more than the luteal phase
- Thermometers aren’t always accurate. A CE mark and under two years old help
- Temperature rise day is the ‘shift day’; this marks the end of the fertile window
- Temperature changes can’t reveal the day of ovulation as:
- 53% of ovulations happen one or two days before the temperature shift
- 27% of ovulations happen on the day of the first high temperature i
- Double ovulation is possible but must be within 24 hours
- To get pregnant, have sex before the temperature shift

The Cervix
The cervix is the lowest portion of the womb and the gateway from the vagina. It’s more than just a muscular tube and plays an essential role in helping women get pregnant and maintain healthy pregnancies. The shape and the type of mucus released from glands in the cervix walls control access to the womb.

By Henry Vandyke Carter
Sex hormones released from the ovaries alter the shape and performance of the glands in the cervix:
- During the infertile parts of the cycle (and in pregnancy), the cervix is closed, and a mucus plug forms that prevent bacteria from entering the womb. The mucus keeps a baby safe in the womb and controls access to the womb after the ‘fertile window’ of the cycle
- After the period, the cervix stays open, and it becomes increasingly “sperm-friendly” as ovulation approaches. Fertile mucus helps sperm make their way to an egg after its release from the ovary
- These changes in the cervix shape and mucus let women check how fertile they’re likely to be
Cervical mucus
- Special glands in the cervix wall produce different types of mucus across the month
- The amount of mucus varies from person to person
- Girls usually produce more mucus than older women
- A ‘cone biopsy’ can remove some or all of these glands, reducing mucus production
- Fertile or transitional mucus is pretty much essential to help sperm reach eggs in natural pregnancies
There are three phases to mucus production, but some women may not recognise them all. It’s easiest to check the mucus by wiping with some paper or by feeling at the cervix opening:

1) Infertile mucus is present at the start of cycles (after the period) and after ovulation:
- It feels dry
- There’s no visible mucus

2) Transitional mucus marks the beginning (and end) of the fertile phase:
- It feels moist or sticky
- Scanty, thick, white, sticky, creamy or yellowish mucus that usually gets thinner
Transitional phase: Sticky, thick, white, creamy, milky, slightly stretchy

3) Fertile mucus is present for a few days before ovulation and possibly for a day after. High estrogen levels can make it 98% water:
- Feels wet, slippery or moist
- Profuse, stretchy (like raw egg white) or very thin, transparent and slippery
Start of fertile phase: Stretchy, white/transparentVery fertile phase: Very stretchy, transparent, watery, abundant
The four different types of fertile mucus have various functions:
- They protect the sperm from the hostile pH of the vagina
- They encourage sperm to swim from the vagina to the womb
- They supply energy to the sperm
- They filter abnormally shaped sperm
As estrogen levels rise in the follicular phase, there‘s a gradual change from infertile (1) to fertile mucus types (2 & 3), and the mucus quickly reverts to type 1 after ovulation. The last day of high-quality mucus is the “peak mucus day”, and it’s usually the day of ovulation.
Additional information
- Fertile mucus doesn’t indicate ovulation as eggs aren’t always released (see LUFS)
- Infections or semen are sometimes mistaken for fertile mucus
- Brown-red mucus or spotting after sex at mid-cycle can signify high fertility, especially when there are very high oestrogen levels. (Spotting after sex can also indicate unwanted changes in cervical cells, but it’ll happen in less fertile phases of the cycle too)
Cervical shape and position
Checking shape and position is a more challenging alternative to checking mucus and is usually done when:
- There’s difficulty recognising the mucus
- There’s no clear mucus pattern
- Surgery has reduced mucus production
Finding the cervix
The best position is usually squatting or sitting on the toilet. Using the abdominal muscles to push down helps; it usually takes a while to find the cervix and recognise changes. It’s most accessible in the luteal phase and varies between feeling like:
- The tip of your nose: hard in the luteal and non-fertile follicular phase
- Your chin and softer in the fertile follicular phase
Typical cycle patterns
Infertile phase:
- The cervical opening is closed
- The cervix is hard and protrudes into the vagina, and is easier to feel
Transitional phase:
- The cervical opening opens slightly
- The cervix becomes softer and becomes shorter and higher in the vagina
Fertile phase:
- The opening (Os) is open
- The cervix is soft and high in the vagina
- The cervix is difficult to reach and feels wet or slippery with type 3 mucus
Lubricants
Lubricants can reduce conception rates. Pre-Seed, canola, mustard, and baby oils don’t seem to harm sperm, but Astroglide, KY products and sesame oil lubricants are known to reduce sperm motility. ii
ii In vitro effects of coital lubricants and synthetic and natural oils on sperm motility’ RS Sandhu, et al. Volume 101, Issue 4 , Pages 941-944 Fertility and sterility, 2014