The “standard semen sample” is the first (and only) test that most men have for their fertility. While it doesn’t test to see if a man’s sperm can actually create a healthy pregnancy, it does check the crucial factors that (usually) indicate if a man is able to father a child naturally:
- Volume of semen
- Concentration of sperm
- Total number of sperm
- Percentage of live sperm
- Number of mobile (and forward-moving) sperm
- Sperm shapes (morphology)
- The pH
- Presence of white blood cells (WBC) and ‘round cells’ (immature sperm cells without tails)
- The presence of anti-sperm antibodies (not always)
- The testing also involves checking:
- Liquefaction (how quickly it turns into liquid)
- Appearance
- Sample viscosity (stickiness)
- Debris in the sample
- Agglutination (clumping)
Why Test
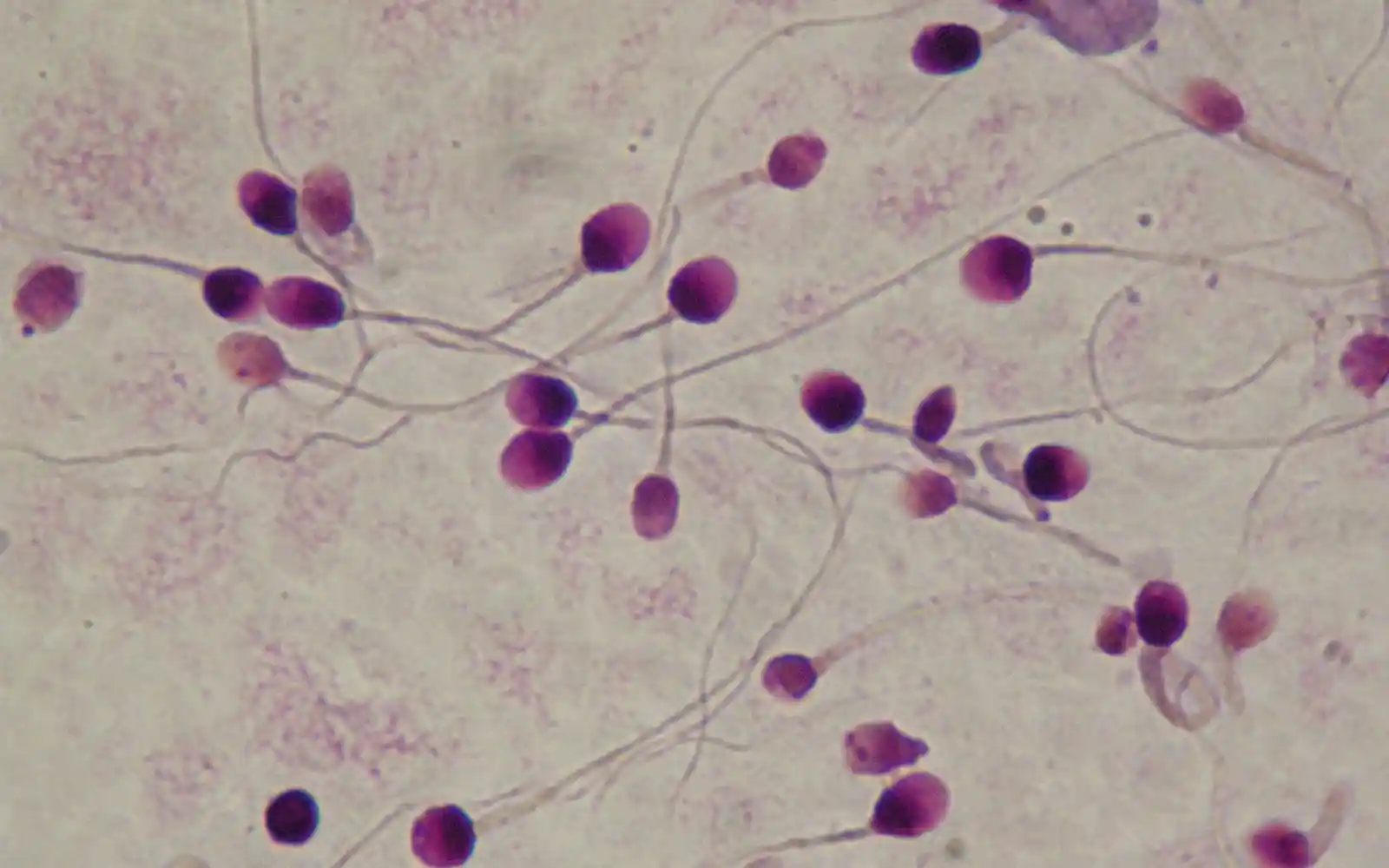
It’s common for many sperm in semen samples to have significant defects, including abnormal heads and tails and few sperm in normal samples are likely to reach eggs. Sperm are made in stages, so abnormalities can indicate where problems with their development occur. It’s really important for couples to have a recent semen sample as
- The World Health Organisation (WHO) reports that 20 – 30% of couples with infertility involved the man ¹
- In fertility clinics, 66% (of 154,412) in-vitro fertilization (IVF) cycles in the USA used intra-cytoplasmic sperm injection (ICSI) in 2011 ²
Although some men are uncomfortable having their semen tested, it provides a clearer fertility picture for a couple, so it’s possible to:
- Diagnose a couple’s fertility more accurately
- Test for any problems the man may have
- Treat more appropriately
- Avoid unnecessary investigations and/or treatments for the woman
The WHO updated its semen reference guide in 2009, creating (per-) ‘centiles’ which show the range within a population of “fertile men”. The men’s partners all got pregnant within a year of trying to conceive.
Each criteria (volume, concentration etc.) is divided into percentages of the ‘norm’ to create a reference framework similar to how a child’s age, weight and height show their position in the general population:
- The 5th centile is the lower limit of “normal”
- The 50th centile is average
- The 95th centile is the upper limit of “normal”
Table 3: Semen values from “fertile men” whose partners got pregnant in the last year (WHO 2009)
Understanding the 2009 WHO references for a fertile man
Volume: The average volume is 3.7 ml, but over 1.5 ml is ‘normal’.
Concentration: The average is 73 million/ml, but over 15 million/ml is ‘normal’.
Motility: The average is 61 %, but over 40 % is ‘normal’.
Morphology: The average is 15 %, but a sample with over 4 % normal shape is normal.
Differences between the 1999 and 2009 WHO references for lower ‘norms’:
- Volume: now 1.5ml, but it was 2.0ml.
- Concentration: 15 million/ml is now the ‘norm’, but it was 20 million/ml.
- Motility: now it’s 40%, but it was 50%.
- Morphology: has seen the greatest change as 4% normal-shaped sperm is now acceptable when it was 15%.
Getting the best semen sample:
- Avoid ejaculating for 2 to 5 days (ideally 3) before the sample
- Less than a day reduces the sperm count
- Over 4 days reduces sperm motility
- Avoid alcohol and non-essential drugs on the sample day and the one before
- Samples need assessment within an hour, so they’re usually collected at the clinic
- Make sure to use an approved container
Advice following a poor semen sample:
- Incomplete samples or problems with testing usually merits a re-test in one to three weeks
- Otherwise, a repeat sample is usually done in 3 months to allow a new batch of sperm to grow
- Abnormal morphology or other irregularities generally merits another test in four to twelve weeks
- If things haven’t improved by then, re-testing in another three months is standard
- With “unexplained infertility”, couples experiencing recurrent ART failure or miscarriage, we recommend additional sperm tests as the next course of action
Examples of semen samples
Examples of semen samples help to explain why standard semen tests are essential, and they can indicate if a man has problems in his testes or tubes and the issue involved. The symbol < means “less than” and > is “more than”.
Sample 1.
|
Patient’s values |
WHO 2009 |
|
| Duration of abstinence [days] |
3 |
2 to 5 |
| Time for ejaculation [mins] |
40 |
<60 |
| Macroscopic examination | ||
| Volume (ml) |
4.1 |
>1.5ml |
| Appearance |
Normal |
Normal |
| Liquefaction |
Complete |
Complete |
| pH |
8.0 |
7.2 – 8.0 |
| Viscosity |
Normal |
Normal |
| Debris |
Not significant |
|
| Agglutination |
None seen |
|
| Motility (% spermatozoa) |
|
|
| (a) Rapid progression |
45 |
>32% |
| (b) Slow progression |
17 |
(a) + (b) > 40% |
| (c) Non-progression |
4 |
|
| (d) Immotile |
34 |
|
| Vitality (%) |
>50 |
>58% |
| Antisperm antibodies |
|
|
| MAR test for IgA |
<10 |
[<10%] |
| MAR test for IgG |
<10 |
[<10%] |
| Concentration [x 10^6/ml] |
|
|
| Count/ml |
37 |
>15 |
| Total count in sample |
152 |
>39 |
| Other cells [x 10^6/ml] |
|
|
| Round cells |
0.3 |
<5 |
| Leukocytes (WBC) |
Not seen |
<1 |
| Morphology [%] |
|
|
| Normal |
15 |
>4% |
| Abnormal |
85 |
|
| Head defects |
85 |
|
| Mid-piece defects |
12 |
|
| Tail defects |
4 |
|
| Cytoplasmic droplets |
1 |
|
| Teratozoospermia Index [TZI] |
1.2 |
<1.6 |
This sample is within the normal range.
Sample 2.
|
Patient’s values |
WHO 2009 |
|
| Duration of abstinence [days] |
3 |
2 to 5 |
| Time for ejaculation [mins] |
60 |
<60 |
| Macroscopic examination |
|
|
| Volume (ml) |
5.8 |
>1.5ml |
| Appearance |
Gel bodies |
Normal |
| Liquefaction |
Partial |
Complete |
| pH |
8.0 |
7.2 – 8.0 |
| Viscosity |
Normal |
Normal |
| Debris |
Not significant |
|
| Agglutination |
None seen |
|
| Motility (% spermatozoa) |
|
|
| (e) Rapid progression |
59 |
>32% |
| (f) Slow progression |
12 |
(b) + (b) > 40% |
| (g) Non-progression |
5 |
|
| (h) Immotile |
24 |
|
| Vitality (%) |
>50 |
>58% |
| Antisperm antibodies | ||
| MAR test for IgA* |
<10 |
[<10%] |
| MAR test for IgG |
<10 |
[<10%] |
| Concentration [x 10^6/ml] | ||
| Count/ml |
33 |
>15 |
| Total count in sample |
128 |
>39 |
| Other cells [x 10^6/ml] | ||
| Round cells |
6.2 |
<5 |
| Leukocytes (WBC) |
1.9 |
<1 |
| Morphology [%] | ||
| Normal |
1 |
>4% |
| Abnormal |
99 |
|
| Head defects |
99 |
|
| Mid-piece defects |
25 |
|
| Tail defects |
18 |
|
| Cytoplasmic droplets |
1 |
|
| Teratozoospermia Index [TZI] |
1.44 |
<1.6 |
This sample is abnormal, with indications of an infection or inflammation. The semen volume and numbers of sperm are fine, but it contains many white blood cells (WBC), and 99% of sperm have abnormal heads. The possible causes are:
- High oxidative stress levels
- Varicocoele
- Heat exposure
- Environmental toxins
- Ageing sperm
- Hypo-osmotic stress
- Genetic defects
The presence of the white blood cells indicates the heat and oxidative stress are almost certainly coming from an infection, and a course of antibiotics is needed.
Interpretation of semen samples
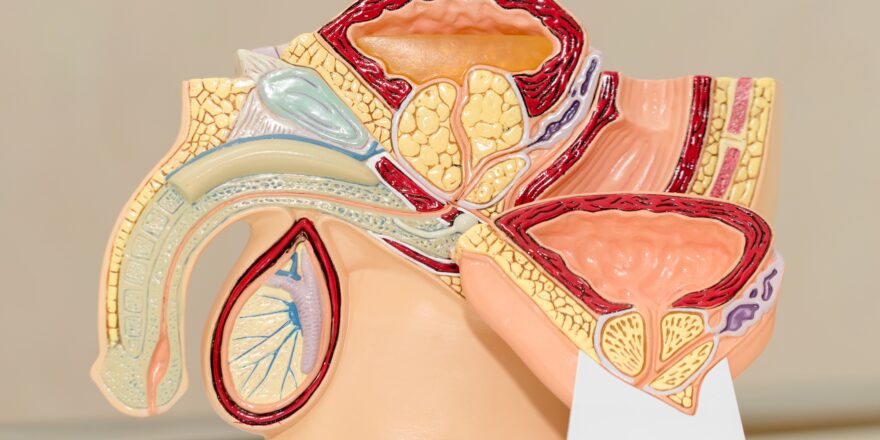
Abnormalities in semen samples can indicate the cause of a fertility problem and where the problem lies. The article on sperm and male organs is a helpful reference.
| Semen sample abnormality | Indicators to the clinician |
|---|---|
| Appearance and volume | A disease of the prostate or the genital tract |
| Liquefaction | Prostate or seminal vesicle dysfunction |
| Volume, pH, appearance, debris, viscosity and leukocytes | Infection or inflammation of the accessory glands |
| Agglutination, MAR test*, motility | Immune-based infertility |
| Count | Dysfunction of the hormone system, exposure to toxins, genetic defects |
| Count, volume, pH | Retrograde ejaculation, dysfunction of the genital ducts, some inherited disorders |
| Count, motility, progression, morphology | Fertility problems |
| Motility | Varicocoele, not ejaculating for too long, infection, inflammation, issues with the genital ducts, anti-sperm antibodies |
| Morphology – which can indicate specific factors | Varicocoele, abnormal sperm development, genetic defects, heat exposure, environmental toxins, ageing sperm, hypo-osmotic stress |
*The MAR test is the “mixed antiglobulin reaction” test used to diagnose immune-based infertility
[2] www.hfea.gov.uk. ‘Fertility treatment in 2010’